More Baby Links
-
March 21, 2007
The Birth of Kathryn
I went for my 38-week appointment on Wednesday, January 24 and was still at 1 centimeter dilated and 50% effaced, no change from the previous week. My doctor went over the plan for what would happen induction-wise if I went late, so I wasn’t expecting much to happen soon. But, I also knew things could start happening at any moment.
On Friday, January 26, I started feeling more of a wetness during the late afternoon/early evening hours, so I began to suspect that my water might be leaking. I’d also started to get some bloody show during the day, enough for a pantyliner. But, I wasn’t convinced enough to call the doctor about it. My husband and I went out that night, stopping to get some litmus paper at a hobby store so I could check if the fluid was basic, which would indicate it was indeed amniotic fluid. (Yes, I’m a dork for getting the litmus paper, but hey, it was cheap!)
We went out to dinner and got home around 10 p.m. and I checked the pH, but it wasn’t showing up as basic, so it didn’t appear to be amniotic fluid. I just figured my discharge was starting to change in preparation for labor. Soon after we got home, I had quite a bit of diarrhea, which was yet another sign (especially looking back) that labor was going to start soon. Around 11 p.m., I started getting really strong, constant menstrual-like cramps in my lower back that sometimes were in my lower abdomen, as well. I knew from reading that this is often how labor starts, and since I hadn’t had any cramping during pregnancy, I really started to suspect something was up. I went to bed around midnight that night and started getting mild contractions during the night, but nothing major.
I woke up at 6:30 a.m. on Saturday, January 27, and my husband and I dropped off the dog at 7:30 for his previously scheduled grooming appointment. I let them know that I was likely in early labor and checked to see if we could board him there if it turned out I really was in labor. They said that wasn’t a problem. (So glad we had the appointment for that morning!) My husband and I got home around 8 a.m. and the contractions, which were mostly in my lower back, were definitely painful. I wasn’t 100% sure this would be the real thing, but I went back to bed to get some rest just in case it was. I had to take my heating pad to bed because my back hurt so much from the contractions, which were about 15 seconds long and probably 8-10 minutes apart at this point (though we weren’t timing them quite yet).
I slept until about 10:30 a.m. and got up. We started timing contractions around 11 a.m., and within an hour, they were 3-4 minutes apart and lasted about 45 seconds. We decided to get ready to go to the hospital. I took a shower while my husband finished packing our last-minute items. By this point, my contractions were painful enough that I had to stop whatever I was doing in order to breathe through them. Leaning over onto all fours so my belly was hanging helped take some of the pressure off. The pains were still in my lower back mostly and sometimes wrapped around to my lower abdomen. I never really felt any contractions high up.
We left for the hospital around 1:30 p.m. and arrived at 2 p.m. We went to labor and delivery and got checked in; then they took me to the labor and delivery room. I changed clothes, used the bathroom one last time, then was asked a ton of questions (mostly health/pregnancy related) by the nurse. They checked me internally and said I was still only 2 to 3 centimeters dilated and about 90% to 100% effaced.
Around 3 p.m., they were ready to put in my IV, which was the worst part of the whole thing for me. It took three nurses and four tries to get in an IV–the first three veins blew–and I was bawling from the experience. Around 3:30 p.m., just when I was filling out my consent forms for the epidural, they injected Stadol into my IV to help take the edge off the contractions, which were becoming more painful, though staying at about the same frequency. I felt the Stadol nearly immediately, as the words on the pages in front of me quickly started running together. I was really surprised by how fast it took effect. It didn’t really take away the pain (I still had to breathe through the contractions), but it definitely made me care less about the pain!
At 4:30 p.m., the anesthesiologist (thanks, Dr. Bennett!) came in to administer my epidural. (I was already pretty sold on the epidural beforehand, and knew with certainty I would get it once I felt those early contractions.) My husband had to leave the room, so he took that time to call my parents, who wanted to come to the hospital, and his family, who all live out of town. (We wanted to wait until I got the epidural since we didn’t want to tell them I was having the baby and then have it be a false alarm.)
I was still under the effects of the Stadol when I had the epidural inserted, so I think that helped relax me. The numbing shot kind of stung at first, but I didn’t feel any pain after that. I could feel the catheter being threaded in, but it didn’t hurt. They also sent a small electrical shock down my left leg to ensure proper placement, but that didn’t hurt either…just a weird sensation. From start to finish, the procedure took about 10 minutes. My epidural took effect immediately, and I didn’t feel any contractions from that point on. My torso was very numbed, but I could still feel my legs for the most part and could even move them quite a bit. It was weird because I had the sensation of itching sometimes on my upper legs, but scratching didn’t help make it go away!
The nurses had a hard time finding my contractions on the external contraction monitor, so they ended up putting in internal monitors for contractions and for the baby’s heart rate once I had the epidural. They also inserted the catheter at this time, which I could feel, but it didn’t hurt.
My doctor wasn’t on call that weekend, so I met one of his practice associates when he came in to check on me around 5 p.m. I really ended up liking him a lot…he had a good sense of humor and was just real laid-back. He checked me around 5 p.m. and I was only at about 4 centimeters and 100% effaced. He also broke my water at that point, which I couldn’t feel, but I did feel the warm sensation of the gush when it came out.
About 5:15 p.m., the blood pressure of both me and the baby plummeted from the epidural, and my temperature dipped quite a bit, too, and I started shivering. I was still feeling the effects of the Stadol, but I do remember them inserting blood pressure medicine into my IV a couple different times in order to stabilize me. They also had me lie on my left side and gave me oxygen for about an hour. I came really close to vomiting at that point and gagged a few times but managed to avoid actually throwing up. They finally got the vitals looking good for both of us and then started a pitocin drip in order to really get the contractions going. My parents arrived around 6:30 p.m. and chatted with us while I labored.
Around 8 p.m., the nurse told me to let them know if I started getting a sensation of pressure, especially in the rectal area. About five minutes after they mentioned that, I started getting that exact pressure and called in the nurse. The doctor came in again to check me around 8:15 p.m. and said that I was fully dilated and it was about time to start pushing. I was actually kind of surprised because I figured it would take longer before I started pushing. My parents went to the waiting room since I wanted it to be just me and my husband for the delivery, and the nurse got things ready for delivery, including getting the bed adjusted into the right position, getting out supplies, and getting the stirrups in place.
I started pushing around 8:40 p.m. In the delivery room were just me, my husband, the doctor, and one nurse. My epidural was still turned on, but I could feel some pressure at the start of each contraction. The doctor did good with telling me how to push. My first couple pushes weren’t great, but after he corrected me and told me how to make it better, my pushes were more effective from then on. We did three pushes on each contraction, with either my husband or the nurse counting for me. The doctor would start talking/joking about random things in between contractions (and sometimes during contractions! LOL), like my career field and state politics, and I really think that helped distract me when I needed it.
A couple times, though, the other three got into their conversation so much that they forgot to finish counting for me. I pushed as long as I could, then jokingly yelled, "Thanks, guys, you stopped counting!" At one point, the doctor asked if I knew what the vacuum was and started going over pros and cons of using it. At the next contraction, apparently I pushed even better than I had been, because he said, "Yep, mentioning the vacuum always makes them push better." Perhaps not a sense of humor for everyone, but he really was amusing.
My husband was able to be both by my side holding one of my legs and could see all of what was going on. (This was fine with me. I’d told him beforehand that it was completely up to him regarding how much he wanted to see himself.) He was fascinated by it all, and I’m actually glad that he was so into it. About 20 minutes into pushing, I suddenly started getting the overwhelming sensation that I was going to throw up, so they got the bedpan for me. I threw up just once (mostly just water since I’d purposely not eaten much that day in anticipation of labor and knowing that vomiting isn’t an unusual occurrence) and felt better after that. Before my last couple of pushes, the doctor went ahead and put on his delivery scrubs, and they called in the baby nurse, who would take care of the baby once she was born. I asked to reach down and touch her head once it was sticking out, and I’m glad I got to do that. Pushing to get the rest of the head and shoulders out hurt a little bit (but still not as much as the stupid IV hurt!).
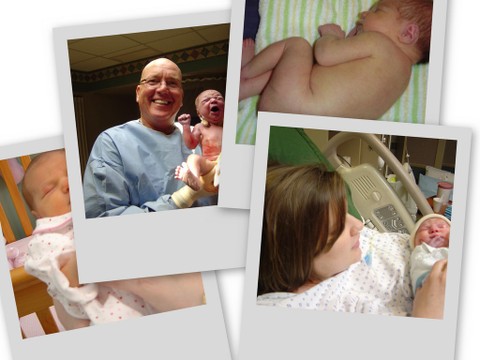
Kathryn Alexandra was born at 9:09 p.m., after pushing for about 30 minutes, and weighed in at 6 pounds, 11 ounces and 19 inches long. She had a rash on some of her face and most of her body, so they wanted to take her to the intake nursery soon in order to make sure it was nothing to worry about. They got her cleaned up and then I got to hold her for only about 10 minutes before they took her. They had my parents come in from the waiting room so they could see her before taking her. I ended up with no episiotomy, and just one minor first-degree tear that did not require stitches. We’d done perineal massage at the recommendation of my doctor ever since my 36-week appointment, so I’m not sure if that’s what helped, but it certainly couldn’t have hurt.
My husband cut the cord (he was unsure if he wanted to, but the doctor had convinced him to do it and he later said he was glad he did), and then the doctor delivered the rest of the umbilical cord and placenta, saying, "And now you are officially not pregnant any more" when it came out. I was under the impression that delivering the placenta took longer, but it was fully delivered within just a few minutes of Katie being born. The doctor put it into a bowl and showed it to my husband then inspected it before setting it down, but I asked to see it, too, since I really was curious. It was turned inside out, but the doctor turned it back out for us so we could see what it looked like in utero. Yeah, it was kind of gross, but I figured I don’t have many opportunities to see something like that, so I might as well! I’m really glad I did. I believe they said Katie’s APGARs were 7 and 8.
They took Katie to the intake nursery to check her rash (which ended up being fine and was mostly gone by the next day) and to give her a bath and check all of her vitals. My parents and my husband went to watch through the viewing window, and my best friend showed up just as my parents were leaving. They got me cleaned up, removed the epidural catheter, and around 11 p.m. they wanted to see how well I could feel my legs to know if I could be moved yet. I still felt a lot of numbness in the left side of my torso and in my lower back (that numbness lasted most of the rest of the night), but I could hold my weight and walk (with some help) just fine. They moved me to a wheelchair to take me to the mother/baby wing, where I would spend the rest of my time in the hospital.
My husband and best friend carried all of our stuff to the new room and they got set up there while the nurses helped me pee (I really had to pee once I could feel again!). I was able to sit down and get up off the toilet fine, and the nurses cleaned up a lot of the blood and gave me the mesh panties and pads to wear. They also showed me how to squirt warm water after I was done peeing in order to keep things as clean as possible. I walked back to the bed mostly on my own with some steadying from the nurse; they were surprised by how much I could walk on my own at that point.
I got back in bed and visited with my best friend while my husband left the room to make phone calls to family and friends with the good news. They started me on two bags of pitocin in order to get my uterus to shrink back, and the nurses came in periodically to check and massage my uterus and keep an eye on my temperature (I’d developed a fever at the end of labor) and blood pressure. My best friend left around 12:30 a.m. and my husband and I just sat and talked for a bit while we waited for them to bring Katie to our room.
She finally came around 2 a.m.–the first time I’d seen/held her since the short time I had her after the birth. We tried breastfeeding immediately, but it was kind of frustrating at first. It felt like everything I’d read about what to do went out of my brain, and of course she didn’t know what to do immediately, either. By the second day, that got easier, but it was certainly frustrating those first couple times. It also didn’t help that I was so tired and just not in the right frame of mind to be patient with breastfeeding, so I decided we’d get a fresh start the next day. We sent her back to the nursery around 4 a.m. so we could get a few hours of sleep. My bleeding was still really heavy at that point, but less than it was right after delivery. It was more manageable by the second day and much like period bleeding after that.
We had Katie in our room all day on Sunday, January 28. I was definitely sore in the crotch, like someone had kicked me hard there, but I imagine it would have been worse if I’d had tears or stitches. Still, getting in and out of bed really hurt. My husband did all of the diaper changes, and feeding went better that day. My best friend and her mom came to visit us that afternoon after church, and the whole day felt like a parade of people who came into our room, one after another…nurses obviously to check on us, but then the hospital photographer, the lactation consultant, the pediatrician, the on-call obstetrician, the birth certificate/Social Security person, etc. I finally got to take a shower around 8 p.m. that night and felt a lot better after that. My best friend came back later that night with her fiance to visit and stayed for about an hour. We sent Katie back to the nursery around 10 p.m. so we could get some rest (with instructions to bring her back during the night when she needed to be fed, which I did around 1:45 a.m. and 4:30 a.m.). My husband and I took a walk around the halls for a few minutes, which was the only time I got out of the room since I was so sore when I walked.
On Monday, January 29, they brought Katie back to our room around 8 a.m. and we waited to be discharged, which they were hoping to do around noon. The pediatrician came and gave his okay to discharge Katie (though we had to take her back to the doctor two days later since she looked jaundiced), but we were still waiting on my obstetrician to come talk to me and give me the okay to leave. We thought he would come while doing rounds before his office hours, but he never came and the nurses didn’t know where he was.
We gathered up our stuff and watched TV while waiting for him. He finally came around 1:30 p.m. and sat down to talk with me. He said he’d been doing a c-section that morning, then had another delivery in the late morning, on top of keeping up with his office appointments, too, so at least there was a good reason for why he was later coming to see me. He asked me how things went, and I said that everything went way better than expected and that the IV was the worst part for me. I said that maybe it was a good thing hearing everyone’s horror stories because maybe that made things better for me!
He started going over instructions on care for my stitches, but I told him that I hadn’t had any stitches. He looked surprised, checked my chart, and said, "Wow, you’re right." I know it’s not the norm to not need stitches, so I really do count myself lucky there. I started asking a few questions about exercise and some other things, and he said that the only rule I had was that intercourse and tampons were forbidden for six weeks, but other than that, I could proceed as I normally would. He told me to continue my prenatal vitamin for as long as I was nursing, and to keep up with my iron supplement for about three months.
All in all, I really think things went extraordinarily well. From the start of the initial cramping, my labor was technically about 22 hours, but it seemed like less than that since my real contractions didn’t start until the next morning, and I delivered only seven hours after arriving at the hospital. I was prepared to push for a lot longer than 30 minutes, since I know it’s common to push for an hour or two (unlike what you see on TV and in the movies!), so I’m very glad that wasn’t the case. I really don’t think I could have asked for a better delivery, despite the few unpleasant parts about it.
Deanna is a copy editor who lives in Kentucky with her husband, daughter, golden retriever, and two cats. You can read her parenting blog "And Baby Makes Three" here.
No related posts.
Posted by Black Belt Mama on March 21, 2007 in Gimme the Drugs | Leave a Comment
Comments
Submissions
Do you have a birth story you would like to share? Please see the submission guidelines.
Email MeHelp Promote the Site
A blog is born
Copyright
© Copyright 2006-2010 blackbeltmama dot com ALL RIGHTS RESERVED-
Recent Posts
Categories
- Au Naturale (10)
- Gestational Diabetes (2)
- Gimme the Drugs (6)
- Give me a C (section) (3)
- Induction-The Lease is Up (6)
- Submission Guidelines (1)
- VBAC (1)
Baby Links
Archives
- December 2007 (1)
- May 2007 (2)
- March 2007 (2)
- February 2007 (1)
- December 2006 (1)
- September 2006 (2)
- August 2006 (6)
- July 2006 (8)